normal bilirubin levels in newborns chart in india
Staff Practice Indian Pediatrics 2002; 39: 30-42 No conjugate Hyperbilirubinemia in newborns: Current Perspective Ramesh Agarwal and A.K. Deorari From the Neonatal Division, Department of Pediatrics, All India Institute of Medical Sciences, New Delhi 110 029, India. Correspondence to: Dr. Ashok K. Deorari, Additional Professor, Indian Institute of Health, New Delhi 110 029, India. E-mail: Cytericity in the newborn is quite common that affects almost 70% of term and 80% of premature newborns during the first week of life. Luckily, most of the time this is a physiological event resulting from increase of bilirubin charges due to breakdown of red blood corpus (RBC); defective, conjugation and excretion by immature liver; and increase of the whole-hepatic circulation. Neonatal hyperbiliubibinemia also known as pathological jaundice results from increased production and limited removal of bilirubin during the initial days of the newborn period. This occurs in almost 5 to 25% of the newborns(1-3). The common causes include sepsis, G6PD deficiency, prematurity, blood group the incompatibility and most are idiopathic. Less common causes include polycytemia, extravagation and oxytocin infusion during work(1,2). Newborn brain is susceptible to toxicity bilirubin not conjugated resulting in "Kernicterus" or "bilirubin" Induced brain damage" (BIND). A. Bilirubin Physiology 1. Source of production The bilirubin is derived from the degradation of the hema proteins present in hemoglobin, myoglobin and certain heme contains enzymes. Three quarters of bilirubin come from hemoglobin catabolism. A gram of hemoglobin results in the production of 34 mg bilirubin. A normal term of the newborn produces about 6-10 mg/kg/day bilirubin that is almost 2 to 3 times compared to adults. 2. Metabolism Bilirubin is intended for blood transport. This bilirubin tied does not enter the central nervous system and is Not toxic. Upon reaching the liver, only bilirubin enters the liver cell and he's tied to ligandin, which helps transport him to the site Conjugation. The conjugation occurs with glucuronic acid to produce mono and dilucuronides that are soluble in water. The conjugated bilirubin is transported with bile to the intestine. The intestinal bacteria reduce this to Estercobilin, who excretes with feces. In the intestine of the newborn sterile, there is an enzyme called beta-glucuronidase, which converts bilirubin glucuronide in the unwoven bilirubin that is reabsorbed in the circulation. This is called whole-hepatic circulation and is particularly important in infants who are not orally fed from birth. With the introduction of food, bacteria destroy this enzyme. 3. Bilirubin encephalopathy La bilirubin combines with albumin in molar concentration (a gram of albumin binds to 8.5 mg of bilirubin). This the bilirubin linked to the albumin is transported to the liver for conjugation and excretion. The bilirubin tied to the albumin cannot cross the blood intact. cerebral barrier (BBB) but once the bilirubin sites in the albumin are saturated, bilirubin free, appears in serum. This free bilirubin can cross BBB and produce bilirubin brain damage. In cases of insult to the BBB, even the bilirubin linked to the albumin can get access to the central nervous system. Once in contact with neurons, additional damage to neurons depends on availability of hydrogen ion. Bilirubin normally exists as a bianion and combined with hydrogen ions to form bilirubin acid (BH2), that precipitates neurons causing damage. Other theoretical states that bilirubin is combined with a hydrogen ion and this molecule positions in itself between the lipid bicapa of the membranes. This move. has surfactant like the property and changes the mem-brane ion function channels that produce early manifestation of bilirubin encephalo-pathy(4). This step is reversible in the intervention thus explaining reversibility of early bilirubin encephalopathy. However, if acidosis persists then BH2 is formed resulting in permanent neuronal damage. B. Assessment of jaundices Clinical criteria Clinical trial is widely used and uses principle that clinical jaundice becomes evident in the face followed by a downward progression while increasing in intensity. The evaluation of jaundice must be made in the natural light. The octopus the finger or thumb is pressed on the baby's skin, preferably on a bony part, until I blink. The underlying skin is noticeable for the yellow color. The excess of jaundice detected gives an approximate estimate of serum bilirubin (Table I). Once bilirubin levels are more than 15 mg/dl, results in plant and palm stains. Serum bilirubin The estimate should be done through laboratory tests to document bilirubin levels for proper management of neonatal jaundice. Table I_Criteria to calculate clinical indexes Body area bilirubin range (mg/100 ml) Cara 4-8 upper trunk 5-12 Baoul and thighs 8-16 Armrest and lower legs 11-18 Palm trees and soles " C. Prediction of hyperbilirubinemia In recent years, many efforts have been made Predicting babies will likely develop neonatal hyperbilirubinemia. Fiable Predictors can reduce the hospital stay for normal babies, resulting in an early discharge and identification at risk or high-risk neonates develop pathological jaundice. These newborns would need to close monitoring for potential risk of bilirubin-induced brain damage to reduce among healthy newborns who have been released early in the hospital. 1. Universal screen of newborn bilirubins Bhutani et al.(5) created percentile graphics for serum bilirubin in different postnatal ages for direct Coomb term negative healthy and newborn babies in the short term. The researcher concluded that by making sérico bilirubin at an early age (e.g. a 24-36 h), posterior hyperbilirubibinemia in a newborn may be predicted by trace the value in the normogram. If total bilirubin serum (TSB) value at this age is falling into the high-risk area (both 95 percentile) or in an intermediate risk zone (%il zone 40 to 95) then possibilities posterior hyperbilirubibinemia is 39.5% and 6.4%, respectively, when it is falling into low-risk area (less than 40th percentile), when There is no measurable risk. In another study(6) of approximately 500 healthy terms newborns, it was observed that a bilirubin serum 36 mg/dl on the first day of life had a sensitivity of 90% prediction rear TSB 317 mg/dl between 2nd and 5th day of life. In this critical serum bilirubin value, the negative predictive value was 97.9%. No cases with TSB mg/dl in the first 24 hours requires later treatment of phototherapy. In an Indian study(7), a cut of 3.99 mg/dl to 18-24 h was found to have sensitivity and specificity of 67% each for the prediction of later hyperbilirubinemia. If confirmed in other studies, these results suggest that there are a group of babies, that at least even Hyperbilirubinemia is concerned, may not require early follow-up. Pre-Download TSB levels can also alert the pediatrician of these babies that, because their TSB levels fall into high-risk area, require much more careful monitoring and follow-up. 2. Estimate of final carbon monoxide Hemoglobin catabolism results in equimolar formation of CO and bilirubin. Corrected final-mare carbon monoxide air of the room is an indicator of hemolysis and production of bilirubines. An CO high-mareal identifies neonates that are high producers of bilirubin, even before the appearance of hyper-bilirubinemia, and can help pediatrician in rapid identification of neonates at risk hyperbilirubinemia or hemolytic disease (8). 3. Estimate of Transcutaneous Bilirubines Several studies (9,10) have traced demons possibility of prediction of serum bilirubin in neonates by analysis the spectral reflectance of the skin. However, the accuracy of these techniques have been complicated by the variability introduced by the skin pigmentation and dermal maturity; therefore the results of the studies White infants cannot be applicable to the heterogeneous Indian population. A managed transcutaneous bilirubinometer (Bili CheckTM) has been designed to correct these interfered factors; be based about recent studies on the scattered luminosity of human skin. General correlation between measurements of BiliCheck and serum The bilirubin estimate by HPLC is linear (r = 0.91). The measures were independent of gestation, race and ethnicity(11). However, a recent study of our group(12) revealed that the estimate of transcutaneous bilirubin can be useful detection tool, but cannot replace total serum bilirubin parti-cular estimation for babies with bilirubin serum Ø13 mg/dl. 4. Cord Blood Bilirubin Levels High cord blood bilirubin in ABO or not ABO the situation indicates a hemolysis in the uterus. These babies more likely to develop hyperbilirubinemia. A level of cord bilirubin √2.5 mg/dl predicts the development of pathological jaundice (defined as bilirubin √13 mg/dl) with 71% sensitivity and specificity 96%(13). D. Hyperbilirubinemia management in Neonates 1. Newborn in a Healthy Mandate The term healthy newborn means a baby born in equality or more than 37 weeks of gestation, without hemolisi or doctor disease. American Academy of Pediatrics (AAP) has established the Guidelines for the management of jaundice in these babies(14) (Table II). It was believed that bilirubin-induced brain damage (BIND) is unlikely to occur in these babies and therapeutic intervention carries more risk that uncertain risk of hyperbilirrubibinemia in this population. Recently Concern has been expressed over AAP practice parameter: (i) There have been reports(15) of Kernicterus occurs in newborns otherwise healthy, without Identifiable risk factors. Notified babies were commonly blowjobs and often discharged from the hospital soon after birth. (ii) It is based only on visual assessment of jaundice that has its own limitation and variations are known occurs especially when it is not done in appropriate conditions(16). Besides, once. jaundice implies whole body then it is difficult to quantify bilirubin levels. (iii) Time interval specified in The parameter is too long. A total bilirubin (TSB) serum from 8 to 24.1 h and 47.9 h must be treated in the same manner as both values on day two. However, in the first situation, the TSB is above 95th percentile therefore has high risk of posterior hyperbilirubinemia and needs close follow-up while in the subsequent situation it is at low risk zone and probably does not require more action. In short, it can be said the AAP practice parameter is somewhat liberal but from now on until better guidelines are available, the present can be used for management of hyperbilirubinemia in healthy-term babies. Table II__ Management of hyperbilirubibinemia in the newborn of the healthy mandate(14) TSB (mg/dl) Age (hours)a Considerb Phototherapy Phototherapyc Transfusion of exchange if Intensive phototherapy Fallsd Transfusion of exchange and Intensive phototherapy 24 - - - - 25 - 48 312 315 320 325 49 - 72 315 318 325 330 372 317 320 325 330 a. Intial jaundice 24 hours is always abnormal and should be investigated for the cause and may require aggressive management in the form of phototherapy and/or exchange transfusion. b. Individual clinical judgment. c. If conventional lights are not able to lower the TSB, the possibility of hemolytic jaundice should be considered. Intensive phototherapy may have to be used in such situations. Phototherapy can be suspended when TSB levels fall below 15 mg/dl. Routine serum bilirubin estimation to see the rebound is usually not necessary but should be individualized. d. The lack of intensive phototherapy has been defined as inability to observe a decrease in the TSB @ 1-2 mg/dl for 4-6 hours and maintain the levels of the TSB below the exchange range. e. If the baby has high bilirubin levels, put the baby under intensive phototherapy and prepare to exchange blood transfusion. If intensive phototherapy does not reduce the levels of the TSB, blood transfusion should be exchanged. The upper TSB level in a baby from 25 to 48 h can indicate hemolytic disease. 2. Newborn Rh Hemolytic Disease Since a significant proportion of births are still occurs at home, Rh isoimmuniza-tion is an important public health problem in India(1-3). These babies can present as hydrops in birth if the awareness has been severe enough or so rapid increase or Seriously high TSB. Progressive anemia and hepato-splenomegaly are usually present. The peripheral look shows evidence of hemolisi in form of aniso-poikilocytosis, elevated normblasts and fragmented red cells. Babies are usually the positive reticulocyte of Coomb is High. The management of an immunitarian hydrops is a real challenge. Effective management requires a team approach for obstetricians and neonatologists that start from early pregnancy. Detailed discussion management of inmunitary hydrops is beyond the current scope communication. Babies, which are not hydropics, should have TSB and PCV measurement of cord blood in addition to ABO writing and Coomb test. In the case of severe anemia (PCV) partial blood is exchanged transfusion with 50 ml/kg red blood cells packed should be transported out for the rapid correction of anemia. Double volume of blood exchange transfusion is performed if other criteria are met. The TSB should monitoring closely every 8-12 hours and babies should be administered aggressive use of intensive phototherapy(17) (Table III). High-dose intravenous immunoglobulin (IGI) when given early in the course of disease can modify the course of the disease. When given in dose of 0.5-1 g/kg as single dose, reduces hemolisi significantly and minimizes the need for transfusion of exchange and duration of phototherapy(18.19). Developing countries like ours, where Rh iso-inmunization still exists, provide an ideal scenario for conduct a randomized controlled study to show efficiency and safety IVIG therapy in Rh isoimmunized neonates. 3. Incompatibility ABO With decreased incidence of hemolytic disease Rh, The incompatibility ABO has become an important cause of hemolytic jaundice in newborn(1-3). In the blood group, the isohaemagglutin mother (Anti A) and Anti B) of type IgG cross the placenta and destroy type A or B red blood cells of the fetus. These isohaemagglutinas are of class IgG and differ from the usual IgM class isohaemagglutinas (incapable of crossing usually present in the blood (Anti A in blood group B and Anti B in blood group A). It is observed that hemolisi is more pronounced in Babies with blood group 'A' than 'B'. In incompatibility, ABO, hemolisi is generally less severe compared to Rh incompatibility and present most times after 24 hours of age. Pre-sence of setting does does not mean incompatibility, therefore the evidence of hemolisis must be carefully searched by examining the peripheral look and performing I reticulate to count. Coomb's direct test is generally nega-tive(13). The Table IV summarizes the suggested management of ABO incompatibility. Table III__Management of Rh hemolytic Disease of Newborn(17) A. Principles Exchange Blood Transfusion 1. Cord bilirubin 35 mg/dl 2. Cord Hb 10 mg/dl 3. In the event of severe awareness to eliminate antibodies in the baby (suggestion of severe affection, Coomb's indirect titre rose in the mother, positive direct proof of Coomb in the baby). B. Transfusion of later exchange 1. Age (h) TSB (mg/dl) 24 3 10 25-48 3 15 " No. 48 " 3 20 2. When the serum increase rate bilirubin 3 0.5 mg/dl per hour C. Intensive Phototherapy: Indicated at a bilirubin level, which is 5 mg/dl less than blood transfusion exchange. D. Preterm/Low birth weight babies: correspondingly lower values should be used. A level equal to or greater than 0.5 and 1% of the birth weight can be used as a rough guide for phototherapy and blood transfusion exchange, respectively. 4. Other hemolytic conditions Lower blood group incompatibility, G-6-PD deficiency, hereditary spherocytosis, autoimmune hemolytic anemia other causes of hemolytic jaundice. Of these deficiencies, G-6-PD deserves a special mention. G-6-PD deficiency is a common condition India, the incidence varies between 5-20% among different ethnic groups (1.2.20). It is more common in Tribes and Parsis. The jaundice can present at any time during the neonatal period, whether spontaneous or next exposure to oxidative stress. The physiological basis for excess no jaundice has been established in infants with G-6-PD deficiency. Increased breakdown of erythrocytes and reduction of bilirubin glucuronidation caused by defective G-6-PD activity in the hepato-cite may have a role in the pathogenesis(21). It can be severe enough to require exchange Blood transfusion (1,2). All babies who develop hyperbilirrubibinemia should :: A review of the deficiencies of the G-6-PD in family counselling with respect to the avoidance of harmful drugs in later life. Table IV_ Management of ABO Incompatibility Intervention TSB (mg/dl) Phototherapy 315-17 Exchange blood transfusion 20 Use the correspondingly low level for premature babies. 5. Premature babies Bilirubin levels for intervention have been reported before in infants with standard risk and high risk(22). High risk Babies are those who have birth weight of less than 1500 g, hypothermia, asphyxiation, acidosis, hypo-albuminemia, sepsis, meningitis, or administer drugs that have potential to displace the bilirubin of the albumin. In high-risk infants cut for intervention are lower. Like a broad blood transfusion guide exchange was recommended for babies bilirubin level of 1% of body weight in grams, i.e. for a baby with wieght of birth 1700 g bilirubin level for exchange is 17 mg/dl. There is change in the induced bilirubin spectrum brain damage in premature babies with virtual disappearance of kernicterus in modern neonatal units in the West. New evi-dences suggest low bilirubin kernicterus in the 1970s and 1980s, which formed the basis for such a recommendation was probably due to the nature of support and UCIN practices such as the use of sulfisoxozale and benzyl alcohol. In addition, in neuro-development follow-up studies, hyper-bilirrubibinemia has not emerged as a single risk factor for the poor neurological outcome(23). There has recently been a change in management practices hyperbilirubinemia in premature babies in the form of starting intervention at higher levels(24). Table V refers to weight-based cut for Phototherapy and transfusion exchange. These are approximate guidelines. It has been recommended that each baby be individualized for intervention. 6. Restricted baby growth The management of bilirubin is related to the maturity of the hepatobiliary system and, therefore, in deciding the intervention, The gestational age should be taken into account more than the weight. 7. Breastfeeding index Multiple studies in the last two decades have found increased incidence of hyperbilirubibinemia in breast-feeding babies. In of Carvalho et al.(25) reported that the frequency of Food was crucial in the genesis of neonatal hyperbilirubinemia. More Progressive breastfeeding led to a lower incidence of jaundice. These are Researchers also showed that glucose water or water supplementation in breastfeeding infants gives rise to a greater serum bilirubin Concentrations that do not supplement infants(26). Yammauchi et al. reported that infants who breastfeed more often milk and less weight loss(27). The degree of jaundice on the 6th day inverse correlational age with frequency of feeding in the first 24 hours. In a recent study(28) the role of breastfeeding in jaundice that occurs in first week showed a statistically significant positive correlation among patients with TSB ratio12.9 mg/dL and supplementary feeding. Infants did not have a greater frequency of significant hyperbilirubinemia but a very small subpopulation had high bilirubin level. Weight loss was strongly associated considerably hyperbilirubi-nemia and was more pronounced in babies with mixture feeding instead of those in exclusive breastfeeding. A well-designed longitudinal study on the physiological jaundice pattern in optimal Breastfeeding still lacks. But it feels like exaggeration jaundice in breast-feeding babies is due to inadequate ingestion of milk and calories instead of any ingredient in breast milk itself exaggerating jaundice. In babies with optimal breast milk, the pattern should not vary and exaggeration is probably related to non-physical-logic management breastfeeding. So while they manage these babies, frequent and exclusive Breastfeeding should be low in consumption. Table V__ Management of neonatal hyperbili-rubinemia in very low-weight babies at birth Based on the level of Bilirubin (mg/dl)(24) Weight (g) Phototherapy Consider the exchange blood transfusion 500- 750 5-8 12-15 750-1000 6-10 √ 13 1000-1250 8-10 15-18 1250-1500 10-12 17-20 a. These are guidelines; each baby must be individualized. b. As a rough guide, start phototherapy in a well-VLBW baby if bilirubin levels are about 1% of the birth weight and exchange blood transfusion to a higher value of more than 5 g/dl. A sick VLBW baby requires intervention before. 8. Protracted jaundice No firm rules can be framed to define abnormals persistence of jaundice in a newborn. It is common to see newborns significantly jaundiced even 2-3 weeks. Careful review of maternity baby's history and thorough clinical examination Adequate management guide (Table VI). According to AAP practice parameter, these babies should be investigated after three weeks, provided they are free of any disease, not having abnormal physical exam, dark urine or light stools(14). By the way, the most common cause of prolonged jaundice is called ñustmilk jaundice ' (BMJ). These babies can be handled effectively with the continuation of breastfeeding and phototherapy even if the TSB exceeds 20 mg/dl in a term Baby. It is important that you do not stop breastfeeding routinely in these babies, which is of immense benefit to the baby(29). Stop. breastfeeding, even for short duration, will result in anxiety and resulting removal of breastfeeding in the mother and many babies can do not return to exclusive breastfeeding. Besides, this extends to Wrong message about breastfeeding. Guidelines have recently been established established for the management of infants with extended conjugate hyperbilirubinemia (30). E. Therapeutic interventions (i) Blood transfusion exchange Exchange Transfusion (ET) is an effective method lowering very high bili-rubin. Blood transfusion early exchange reverts the brain damage of transient bilirubin(31). Abnormal auditorium evoked chronology in case of neonatal hyperbilirubinemia that persists even after well-connected therapy with neuro-developmental delay at 1 year of age(32). Fresh blood, preferably 72 hours of age are used. For the choice of blood see the table VII. The procedure is performed by a catheter of 5 or 6 F in umbilical vein for a distance where you get free flow of blood. In In addition to the risk of blood birth infection, ET carries a significant risk of vascular accident morbidity, heart complications and biochemical or hematological disorders, although mortality due to procedure itself is very rare (1,3,33). Table VI_Prolonged ictericia Common causes 1. Maternal milk jaundice 2. Extravaded blood, for example, cefalhematoma 3. Persistence of hemolisis 4. Deficiency of the G-6-PD 5. Hipotiroidism Workup • Careful history and clinical examination • Regulate the colostasis (color of stool, direct and indirect bilirubin levels) • Find hemolisis, G-6-PD display • discard hypothyroidism • Extends urinary tract infection (ii) Phototherapy Phototherapy has been found effective treatment of hyperbilirubibinemia in hemolytics, as well as non-hemolytic Adjustments. It has drastically reduced the need for transfusion of exchange. The TSB decrease depends on the dose of radiation, skin area TSB level exposed and initial. The bilirubin not conjugated in the skin converted into water-soluble photoproducts on exposure to light particular wavelength (425-475 mm). These photo-products are water soluble, non-toxic and excreted in intestine and urine. For phototherapy to be effective, bilirubin needs to be present on the skin so not paper for prophylactic phototherapy(24). (a) Isomerization of configuration: Here. bilirubin Z-isomers become E-isomers. The reaction is instant about exposure to light but reversible as bilirubin Get to the bile duct. After the exhibition of 8-12 hours Phototherapy, this constitutes about 25% of the TSB, which is not toxic. Since this is slowly excreted from the body, so this is not a problem Mecha-nismo for the TSB decrease. (b) Structural Isomerization: This Is an irreversible reaction where bilirubin becomes Lumirubin. The reaction is directly proportional to the dose Photo therapy. This product forms 2-6% of the TSB that is quickly excreted from the body and is primarily responsible for induced phototherapy decline on the TSB. c) Photo oxidation: This is a minor Reaction, where the photoproducts excrete in the urine. Table VII__ Election of Blood for Blood Transfusion Rh iso-immunization: In emergency situations use negative O Rh cells. Ideal is to use negative blood O Rh suspended in AB plasma. The blood group of the baby paired cross, but Rh negative can also be used. ABO Incompatibility: Blood group or types (Rh compatible) with baby. Ideal to use the blood group O (Rh compatible) suspended in AB plasma. Other situations: Cross-Birth Blood Group. Blood volume used: For partial exchange: 50 ml/kg For double volume exchange: twice the baby's blood volume. Types of Light The most effective lights are the ones they have high-energy output near peak adsorption of bilirubin (450-460 nm). Blue special lamps with maximum output to 425-475 nm the most efficient and these do not emit harmful ultraviolet rays. Blue Green light can interfere with the monitoring of cyanosis. Plus, blue light causes nausea, gin and headache to staff working in ICU. The green light causes the erythema and the subsequent tanning of the skin. A combination of two blue and two white tube lights (20 w each) are sufficient to provide an adequate irradiation of 4 to 8 microwatt/cm2/nm. Increase radiation to 10-12 microwatt/cm2/nm a combination of four blue tubes and two whites have to be used. The Radiation should be measured by the fluximeter(34). Fresh day light bulbs ( fluorescent tube light 6-8, 20 W each) with a main peak of 550 to 600 nm and a range of 380 to 700 nm are most commonly used in phototherapy units in our country. These units provide 4-6 microwatt/cm2/nm, when fluorescent tubes are new. With the use of irradiancy is tied to be much lower than required for therapeutic purposes. These units are effective in the treatment of non-hemolytic jaundices in the term and premature Newborns. Occasionally these are not particularly effective in cases of severe or rapidly increasing neonatal jaundice. Remember the lamps should be changed every 3 months or before if the irradian is being monitored. Putting a blue or glass plastic sheet in front of white lamps will not increase the irradiation of the unit in the bluegreen range, but rather decrease. In an attempt to offer intensified phototherapy; Carvalho et al. designed a unit with seven-day fluorescent light tubes placed immediately under the floor of a transparent Plexiglas crib(35). The unit delivered an irradiation of 19 μw/cm2/nm and was as effective as a unit containing special blue fluorescent tube in treatment of non-hemolytic hyperbilirubinemia in infants. Halogen white light (150 W, 21 V) that has significant The output in the blue spectrum is useful for babies under radiant heaters. Opening size (3-20 inches) and mattress distance drive can be controlled. The interior coating of reflective surface of the halogen bulb absorbs most of the infrared rays (IR) (a fan continuously cools it) and a UV Filter in front of blocks of light bulbs harmful UV rays from reaching the baby. The indigenous halogen bulb phototherapy units may lack UV filter and therefore may not be safe for use(34). The recent fiber optic light system provides high-intensity lamp light to a fiber optic pad or blanket. Lighting is transmitted from a halogen lamp source to a fiber optic package contained in a pad in which the baby can lie. These systems have obvious advantages of not requiring eye patch, don't warm the baby; the team is less voluminous than conventional phototherapy equipment and babies can be maintained and nurses while receiving photo therapy. Available studies(36) have shown that fiber optic system is as effective as conventional phototherapy systems in short-term and premature babies. Double surface phototherapy is more effective than the single surface because the average irradiation of the previous is greater(37). Double surface phototherapy can be provided either by special blue light of double surface or by conventional blue Light fiber and subsurface phototherapy. This is convenient. way to offer double phototherapy when it is necessary to reduce the bilirubin level as fast as possible. A new high-intensity nitronic blue light emitting diode phototherapy has recently been tested and found effective in reducing bilirubin by providing much greater irradiation Intensive phototherapy(38). It's a mistake to assume that only because of a Phototherapy unit emits fluorescent light when activated; is necessarily the treatment for the baby with jaundice. In a audit of fetotherapy units in four neonatal centres care in different parts of the country, it was found that only 31% (18/50) units provided an acceptable level of irradiation (39). That's right. imperative that one must periodically verify the irradiation of photo therapy units used to treat pathological jaundice. Phototherapy used for treating pathological jaundice is like giving a medicine. One not. justified in the use of substandard light sources for the treatment of neonatal jaundice. Solar light is relatively ineffective due to low blue content of light. In addition, hyper-piraxia and skin burns can occur in prolonged periods exposure to sunlight. Phototherapy has been used for 50 years and has showed excellent safety track. Recently, the effect of phototherapy on The rate of cerebral blood flow (CBFV) has been reported. Phototherapy increase of average CBFV in all premature babies, who returned to pre-therapy values after discontinued phototherapy only in Non-ventilated babies(4). Even in short-term babies, phototherapy increased CBFV, which returned to the pre-therapy level after the interruption of Phototherapy(41). Phototherapy has been shown to affect the short term behaviour of the term infant, which has been attributed to maternity separation(42). So one should encourage the mother to breastfeed and interact with your baby regularly. In addition, the influences of phototherapy cytokine production by perpheral mononuclear blood cells(43). Phototherapy also has photoxidative effects on intravenous lipids, proteins and drugs such as anphotericin B. F. Drug treatment (i) Fenobarbitone Phenobarbitone long ago used for the prevention of jaundice. Induces glucuronyl transferase enzyme so it improves conjugation and absorption and excretion of bilirubin by liver cells. Although their use has not become the standard of care from now on, there the evidence that phenobarbitone can be useful prevention is increasing measurement, especially in preterms(44), hemolytic setting and in case of extravagant blood. If used in doses of 5-10 mg/kg/day, you may have beneficial effect without significant adverse effects. (ii) High-dose intravenous immunoglobulin Hyperbilirubinemia in Rh and ABO sensitized of the destruction of neonatal red cells covered by transplacental acquired antibodies that causes the destruction of red cells mediated by Fc receptor bearing cells within the reticuloendothelial system. Recent studies have shown that high intravenous dose Immunoglobulin therapy is effective in modifying hyperbilirubinemia in most cases of positive hemolytic anemia of Coomb(18,19). It was. proposed that immunoglobulin blocks Receptors Fc inhibiting this hemolysis and reduction of bilirubin training. Intravenous immunoglobulin is given in doses of 500-1000 mg/kg as slow infusion over 2 hours. The child must be carefully monitored so that it is possible effects with special attention to heart rate and blood pressure. (iii) Protoporphyllins Metalloporfirins are competitive heme inhibitors oxygenase, an enzyme that limits the rate in heme catabolism by reducing this Production of bilirubin. Clinical trials have shown that the tin Mesoporfirins (SnMP) suppresses bilirubin production. The drug has been found to be devoid of greater negative effect, the only transitory being It's very bad. SnMP at a single dose of 6 μmol/kg tested plus effective phototherapy in a group of infants in the short term without hemolytic disease (45). Recently a similar study on the term infants without hemolytic disease also showed the ability to SnMP to abolish the need for phototherapy(46). To date, SnMP remains experimental but seems to have a promise for the future. In conclusion, non-conju management hyperbilirubinemia in newborns has undergone changes based on appearance tests. New approaches to preventing bilirubin brain damage are on the horizon, but phototherapy and blood transfusion exchange are the most used modalities to reduce serum bilirubin levels. Early prediction of "at risk" baby development of significant jaundices is gaining attention and interest Pediatricians. This issue is particularly relevant in the context of the principles hospital discharge policy in developing countries where there is resource shortage. Collaborators: The AKD provided the general framework and concept of the article. He will. act as the guarantor of the paper. RA collected data and wrote manuscript, which was edited by AKD. Financing: None. Competing interests: None. Key messages • Unconjugated jaundice is important problem in newborns. • Hyperbilirubinemia in healthy term Babies can be given according to AAP criteria. There is growth consensus on the use of higher bilirubin levels for intervention in premature babies. • Phototherapy is an effective modality for the treatment of hyperbilirubinemia in non-hemolytic as hemolytic configuration. • Fenobarbitone, intravenous immunoglobulin and Sn-protoporfirins are the pharmacological measures that show Promise. References 1. Narang A, Gathwala G, Kumar P. Neonatal jaundice: Analysis of 551 cases. Indian Pediatr 1997; 34: 429-432. 2. Singhal PK, Singh M, Paul VK, Deorari AK, Ghorpade MG. Neonatal hyperbilirubibinemia: An Analysis 454 cases. Indian Pediatr 1992; 29: 319-325. 3. Bahl L, Sharma R, Sharma J. Ethology of Neonatal jaundice in Shimla. Indian Pediatr 1994; 31: 1275-1278. 4. Cashore WJ. Bilirubin Metabolism and Toxicity in the newborn. In: Fetal and neonatal physiology, 2nd edition. Eds Polin RA, Fox WW. Philadelphia. W.B. Saunders Company, 1998; pp 1493-1497. 5. Bhutani VK, Johnson L, Sivieri EM. Predictive ability of an hour of specific bilirubin predisposition for later significant hyper-bilirubinemia in healthy term and near term newborns. Pediatrics 1999; 103-6-14. 6. Alpay F, Sarici SU, Tosuncuk HD, Serdar MA, Inanc N, Gokcay E. The value of the first day bilirubin measurement prediction of the development of significant hyperbilirubinemia term healthy newborns. Pediatrics 2000; 106: e16. 7. Awasthi S, Rehman H. Early prediction Neonatal hyperbilirubinemia. Indian J Pediatr 1998; 65: 131-139. 8. Stevenson DK, Vreman JH. Carbon monoxide and Production of bilirubines in neonates. Pediatrics 1997; 100: 252-254. 9. Tan KL. transcutaneous bilirubinomy in its entirety Chinese and Malaysian children. Acta Pediatr Scand 1982; 71: 593-596. 10. Jacques S, Saidi I, Ladner A, Oerlberg D. Develop a fiber optic re-election spectrometer to monitor bilirubinemia in neonates. SPIE Proceedings 2975, Laser Tissue Interactions, San José CA, February 1997; p7. 11. Bhutani VK, Gourley GR, Adler S, Kreamer B, Dalm C, Johnson LH. Non-invasive measurement of total serum bilirubin in a population of newborns pre-load multiracial Assess the risk of severe hyperbilirubinemia. Pediatrics 2000; 106: e17. 12. Lodha R, Deorari AK, Jatana V, Paul VK. Non-invasive estimation of total serum bilirubin by multiple wavelength Spectral reflectance in the neonates. Indian Pediatr 2000; 37: 771-775. 13. Simpson L, Deorari AK, Paul VK. Cord bilirubin as pathological icterity predictor – A cohort study (low publication). 14. American Academy of Pediatrics. Practice parameter: Handle of hyperbilirubi-nemia in term healthy Newborn. Pediatrics 1994; 94: 558-567. 15. Maisels MJ, Newman TB. Kernicterus in otherwise healthy, newborn breasts. Pediatrics 1995; 96: 730-733. 16. Moyer VA, Ahn C, Sneed S. Accuracy of clinical trial in the neonatal period. Arch Pediatr Adolesc Med 2000; 154: 391-394. 17. Maisels MJ. Jaundice. In: Neonatology: Patophysiology and Management of the Newborn, 4th edn. Eds Avery GB, Fletcher MA, McDonald MG. Philadelphia, J.B. Lippincott, 1994; p 765. 18. Alpay F, Sarici SU, Okutan V, Erden G, Ozean-O, Gokcay E. High-dose intravenous immunoglobulin therapy in neonatal immune hemolytic jaundice. Acta Pediatr 1999; 88: 216-219. 19. Agarwal R, Seth R, Paul VK, Deorari AK. High intravenous dose of immunoglobulin therapy in the treatment of Rhesus Hemolytic disease. J Trop Ped, April 2002 (In Press). 20. Singh M. Jaundice. In: Watch out Newborn, 5th edn. New Delhi. Sagar Publications, 1999; pp 245-266. 21. Seidman DS, Shildr M, Stevenson DK, Vreman JH. Function of hemolysis in neonatal jaundice associated with Glucose-6-Phos-phate Dehydrogenase deficiency. J Pediatr 1995; 127: 804-806. 22. National Institute of Child Health and Human Development. Random controlled phototherapy test for Neonatal hyperbilirubinemia. Pediatrics 1985; 75 (Supplement): 385-441. 23. Watchko JF, Oski FA. Kernicterus in default newborns: Past, present and future. Pediatrics 1992; 90: 707-715. 24. Cashore WJ. Bilirubin and jaundice in the micropremie. Clin Perinatol 2000; 27: 171-179. 25. De Carvalho M, Hall M, Marvey D. Effect of supplementation of water in physiological jaundice in breast-feeding babies. Arch Dis Child 1981; 56: 569-569. 26. De Carvalho M, Klaus MH, Merkatz MB. Breastfeeding frequency and serum bilirubin concentration. Am J Dis Child 1982; 136: 747-748. 27. Yamauchi Y, Yamanouchi H. The relationship between the variables of accommodation/no room and lactation. Acta Pediatr Scand 1990; 79: 1017-1022. 28. Bertini G, Dani C, Tronchin M, Rubaltelli FF. Does breastfeeding really favor neonatal jaundice? Pediatrics 2001; 107: e41. 29. Gartner LM, Lee K. Jaundice in breastfed infants. Clin Perinatol 1999; 26: 431-445. 30. Yaccha SK. Neonatal consensus reports Coltasis. Indian Pediatr 2000; 37: 845-851. 31. Deorari AK. Singh M, Ahuja GK, Bisht MS, Verma A, Paul VK, Tandon DA. One-year result of serious babies neonatal hyperbilirubinemia and reversible abnormality in the brain stem evoked hearing responses. Indian Pediatr 1994; 31: 915-921. 32. Agarwal VK, Shukla R, Misra PK, Kapoor RK, Malik GK. Hearing brain evokes newborn response hyperbilirubinemia. Indian Peidatr 1999; 35: 513-518. Jindal B, Narang A, Das R. Post transfusion graft against host disease: A recognized entity. Indian Pediatr 2001; 38: 179-183. 34. Agarwal RK, Deorari AK. Neonatal jaundice. Indian Pediatr 1999; 36: 110-112. 35. Carvalho MD, Carvalho DD, Trzmielina S, Lopes JMA, Hansen TWR. Intensified phototherapy with daylight fluorescent lamps. Clin Pediatr 1999; 88: 768-771. 36. Costello SA, Nyikal J, Yu VVH, McCloud P. bili blanket phototherapy system versus conventional phototherapy. A randomized control test in premature babies. J Pediatr Child Health 1995; 31: 11-31. 37. Sarici SV, Alpay F, Unay B, OZcan O, Gokcay E. Double versus individual phototherapy in newborns in the term Significant hyperbilirubinemia. J Trop Pediatr 2000; 46: 36-39. 38. Sedman DS, Moise J, Ergaz Z, Laor A, Vreman HJ, Stevenson DK et al. A new blue light emitting Phototherapy device: A possible randomized controlled trial. J Pediatr 2000; 136: 771-774. 39. Pejaver RK, Vishwanath J. An audit of Phototherapy units. Indian J Pediatr 2000; 67: 883-884. 40. Benders MJ, Van Bel F, Van de Born. The phototherapy effect on the speed of cerebral blood flow in default infants. Biol Neonate 1990; 73: 228-234. 41. Benders MJ. Van Bel F, Vande-BorM. Hemodynamic consequences of phototherapy in short-term babies. Eur J Pediatr 1999; 158: 323-328. 42. Abrol P, Sankarasubramanian R. Effect of Phototherapy on the behavior of the Jaundic neonates. Indian J Pediatr 1998; 65: 603-607. 43. Sirota L, Straussbery R, Gurrary N, Aloni D, Bessler H. Phototherapy for neonatal hyperbilirubinemia affects cvytokine production by peripheral blood mononuclear cells. Eur J Pediatr 1999; 158: 910-913. 44. Kumar R, Narang A, Garewal G. Prophylactic phenobarbitone for neonatal jaundice in babies from 1000 to 1499 grams. XXth Annual Convention of the National Forum of Neonatology, Mumbai, 3-5 November 2000. 45. Kappas A, Drummond GS, Henschke C, Valaes T. Direct comparison of Sn Meso-porfirins, bilirubin inhibitor production and phototherapy in hyperbili-rubinemia control of newborns in the short term. Pediatrics 1995; 95: 468-474. 46. Martinez JC, García HO, Otheguy LE, Drummond GS, Kappas A. Control of severe hyperbilirubinemia in long-term newborns with the bilirubin production inhibitor Sn-Mesoporphyrins. Pediatrics 1999; 103: 1-5. Staff PracticePersonal Practice Indian Pediatrics 2002; 39: 30-42 No conjugate Hyperbilirubinemia in newborns: Current Perspective No conjugate Hyperbilirubinemia in newborns: Current Perspective Ramesh Agarwal and A.K. DeorariRamesh Agarwaland A.K. Deorari From the Neonatal Division, Department of Pediatrics, All India Institute of Medical Sciences, New Delhi 110 029, India. Correspondence to: Dr. Ashok K. Deorari, Additional Professor, Indian Institute of Health, New Delhi 110 029, India. E-mail: From the Neonatal Division, Department of Pediatrics, All India Institute of Medical Sciences, New Delhi 110 029, India. Correspondence to: Dr. Ashok K. Deorari, Additional Professor, Indian Institute of Health, New Delhi 110 029, India. E-mail: From the Neonatal Division, Department of Pediatrics, All India Institute of Medical Sciences, New Delhi 110 029, India. Correspondence to: Dr. Ashok K. Deorari, Additional Professor, Indian Institute of Health, New Delhi 110 029, India. E-mail: Newborn jaundice is quite common that affects almost 70% of term and 80% of premature newborns during the first week of life. Luckily, most of the time this is a physiological event resulting from increase of bilirubin charges due to breakdown of red blood corpus (RBC); defective, conjugation and excretion by immature liver; and increase of the whole-hepatic circulation. Neonatal hyperbiliubibinemia also known as pathological jaundice results from increased production and limited removal of bilirubin during the initial days of the newborn period. This occurs in almost 5 to 25% of the newborns(1-3). The common causes include sepsis, G6PD deficiency, prematurity, blood group the incompatibility and most are idiopathic. Less common causes include polycytemia, extravagation and oxytocin infusion during work(1,2). Newborn brain is susceptible to toxicity bilirubin not conjugated resulting in "Kernicterus" or "bilirubin" Induced brain damage" (BIND). A. Bilirubin Physiology A. Bilirubin Physiology1. Source of ProductionBilirubin is derived from the breakdown of the heme proteins present in hemoglobin, myoglobin and certain heme contains enzymes. Three quarters of bilirubin come from hemoglobin catabolism. A gram of hemoglobin results in the production of 34 mg bilirubin. A normal term of the newborn produces about 6-10 mg/kg/day bilirubin that is almost 2 to 3 times compared to adults. 2. MetabolismBilirubin is intended for blood transport. This bilirubin tied does not enter the central nervous system and is Not toxic. Upon reaching the liver, only bilirubin enters the liver cell and he's tied to ligandin, which helps transport him to the site Conjugation. The conjugation occurs with glucuronic acid to produce mono and dilucuronides that are soluble in water. The conjugated bilirubin is transported with bile to the intestine. The intestinal bacteria reduce this to Estercobilin, who excretes with feces. In the intestine of the newborn sterile, there is an enzyme called beta-glucuronidase, which converts bilirubin glucuronide in the unwoven bilirubin that is reabsorbed in the circulation. This is called whole-hepatic circulation and is particularly important in infants who are not orally fed from birth. With the introduction of food, bacteria destroy this enzyme.3. Bilirubin Encephalopathy The bilirubin combines with albumin in molar concentration (a gram of albumin binds to 8.5 mg of bilirubin). This the bilirubin linked to the albumin is transported to the liver for conjugation and excretion. The bilirubin tied to the albumin cannot cross the blood intact. cerebral barrier (BBB) but once the bilirubin sites in the albumin are saturated, bilirubin free, appears in serum. This free bilirubin can cross BBB and produce bilirubin brain damage. In cases of insult to the BBB, even the bilirubin linked to the albumin can get access to the central nervous system. Once in contact with neurons, additional damage to neurons depends on availability of hydrogen ion. Bilirubin normally exists as a bianion and combined with hydrogen ions to form bilirubin acid (BH2), that precipitates neurons causing damage. Other theoretical states that bilirubin is combined with a hydrogen ion and this molecule positions in itself between the lipid bicapa of the membranes. This move. has surfactant like the property and changes the mem-brane ion function channels that produce early manifestation of bilirubin encephalo-pathy(4). This step is reversible in the intervention thus explaining reversibility of early bilirubin encephalopathy. However, if acidosis persists then BH2 is formed resulting in permanent neuronal damage. B. Assessment of jaundices B. Evaluation of the IndexClinical CriteriaThe cynical judgment is widely used and uses principle that clinical jaundice becomes evident in the face followed by a downward progression while increasing in intensity. The evaluation of jaundice must be made in the natural light. The octopus the finger or thumb is pressed on the baby's skin, preferably on a bony part, until I blink. The underlying skin is noticeable for the yellow color. The excess of jaundice detected gives an approximate estimate of serum bilirubin (Table I). Once bilirubin levels are more than 15 mg/dl, results in plant and palm stains. Serum bilirubin The estimate should be done through laboratory tests to document bilirubin levels for proper management of neonatal jaundice. Table I_Criteria to calculate clinical indexes Body area bilirubin range (mg/100 ml) Cara 4-8 upper trunk 5-12 Baoul and thighs 8-16 Armrest and lower legs 11-18 Palm trees and soles " C. Prediction of hyperbilirubinemia C. Prediction of hyperbilirubinemia In recent years, many efforts have been made Predicting babies will likely develop neonatal hyperbilirubinemia. Fiable Predictors can reduce the hospital stay for normal babies, resulting in an early discharge and identification at risk or high-risk neonates develop pathological jaundice. These newborns would need to close monitoring for potential risk of bilirubin-induced brain damage be reduced among the healthy newborns given early discharge from the hospital.1. Universal Newborn Bilirubin ScreeningBhutani et al.(5) created percentile graphics for serum bilirubin in different postnatal ages for direct Coomb term negative healthy and newborn babies in the short term. The researcher concluded that by making sérico bilirubin at an early age (e.g. a 24-36 h), posterior hyperbilirubibinemia in a newborn may be predicted by trace the value in the normogram. If total bilirubin serum (TSB) value at this age is falling into the high-risk area (both 95 percentile) or in an intermediate risk zone (%il zone 40 to 95) then possibilities posterior hyperbilirubibinemia is 39.5% and 6.4%, respectively, when it is falling into low-risk area (less than 40th percentile), when There is no measurable risk. In another study(6) of approximately 500 healthy terms newborns, it was observed that a bilirubin serum 36 mg/dl on the first day of life had a sensitivity of 90% prediction rear TSB 317 mg/dl between 2nd and 5th day of life. In this critical serum bilirubin value, the negative predictive value was 97.9%. No cases with TSB mg/dl in the first 24 hours requires later treatment of phototherapy. In an Indian study(7), a cut of 3.99 mg/dl to 18-24 h was found to have sensitivity and specificity of 67% each for the prediction of later hyperbilirubinemia. If confirmed in other studies, these results suggest that there are a group of babies, that at least even Hyperbilirubinemia is concerned, may not require early follow-up. Pre-Download TSB levels can also alert the pediatrician of these babies that, because their TSB levels fall into high-risk area, require much more careful monitoring and follow-up.2. High-end carbon monoxide The catabolism of hemoglobin results in equimolar formation of CO and bilirubin. Corrected final-mare carbon monoxide air of the room is an indicator of hemolysis and production of bilirubines. An CO high-mareal identifies neonates that are high producers of bilirubin, even before the appearance of hyper-bilirubinemia, and can help pediatrician in rapid identification of neonates at risk hyperbilirubinemia or hemolytic disease(8).3. Estimate of Transcutaneous Bilirubin Several studies(9,10) have drawn demons possibility of prediction of serum bilirubin in neonates by analysis the spectral reflectance of the skin. However, the accuracy of these techniques have been complicated by the variability introduced by the skin pigmentation and dermal maturity; therefore the results of the studies White infants cannot be applicable to the heterogeneous Indian population. A managed transcutaneous bilirubinometer (Bili CheckTM) has been designed to correct these interfered factors; be based about recent studies on the scattered luminosity of human skin. General correlation between measurements of BiliCheck and serum The bilirubin estimate by HPLC is linear (r = 0.91). The measures were independent of gestation, race and ethnicity(11). However, a recent study of our group(12) revealed that the estimate of transcutaneous bilirubin can be useful detection tool, but cannot replace total serum bilirubin parti-cular estimation for babies with bilirubin serum Levels of bilirbine cord cord radiated bilirubin blood in ABO or not ABO the situation indicates a hemolysis in the uterus. These babies more likely to develop hyperbilirubinemia. A level of cord bilirubin √2.5 mg/dl predicts the development of pathological jaundice (defined as bilirubin √13 mg/dl) with 71% sensitivity and specificity 96%(13). D. Hyperbilirubinemia management in Neonates D. Hyperbilirubinemia management in Neonates1. Newborns in Healthy terms The term healthy newborn means a baby born in equality or more than 37 weeks of gestation, without hemolisi or doctor disease. American Academy of Pediatrics (AAP) has established the Guidelines for the management of jaundice in these babies(14) (Table II). It was believed that bilirubin-induced brain damage (BIND) is unlikely to occur in these babies and therapeutic intervention carries more risk that uncertain risk of hyperbilirrubibinemia in this population. Recently Concern has been expressed over AAP practice parameter: (i) There have been reports(15) of Kernicterus occurs in newborns otherwise healthy, without Identifiable risk factors. Notified babies were commonly blowjobs and often discharged from the hospital soon after birth. (ii) It is based only on visual assessment of jaundice that has its own limitation and variations are known occurs especially when it is not done in appropriate conditions(16). Besides, once. jaundice implies whole body then it is difficult to quantify bilirubin levels. (iii) Time interval specified in The parameter is too long. A total bilirubin (TSB) serum from 8 to 24.1 h and 47.9 h must be treated in the same manner as both values on day two. However, in the first situation, the TSB is above 95th percentile therefore has high risk of posterior hyperbilirubinemia and needs close follow-up while in the subsequent situation it is at low risk zone and probably does not require more action. In short, it can be said the AAP practice parameter is somewhat liberal but from now on until better guidelines are available, the present can be used for management of hyperbilirubinemia in healthy-term babies. (i) There have been reports(15) of Kernicterus occurs in newborns otherwise healthy, without Identifiable risk factors. Notified babies were commonly blowjobs and often discharged from the hospital soon after (ii) It is based only on visual assessment of jaundice that has its own limitation and variations are known occurs especially when it is not done in appropriate conditions(16). Besides, once. jaundice implies whole body then it is difficult to quantify Levels of bilirubin.(iii) Time interval specified in The parameter is too long. A total bilirubin (TSB) serum from 8 to 24.1 h and 47.9 h must be treated in the same manner as both values on day two. However, in the first situation, the TSB is above 95th percentile therefore has high risk of posterior hyperbilirubinemia and needs close follow-up while in the subsequent situation it is at low risk zone and probably does not require more action. In short, it can be said the AAP practice parameter is somewhat liberal but from now on until better guidelines are available, the present can be used for management of hyperbilirubinemia in healthy-term babies. Table II__ Management of hyperbilirubibinemia in the newborn of the healthy mandate(14) TSB (mg/dl) Age (hours)a Considerb Phototherapy Phototherapyc Transfusion of exchange if Intensive phototherapy Fallsd Transfusion of exchange and Intensive phototherapy 24 - - - - 25 - 48 312 315 320 325 49 - 72 315 318 325 330 372 317 320 325 330 a. Intial jaundice 24 hours is always abnormal and should be investigated for the cause and may require aggressive management in the form of phototherapy and/or exchange transfusion. b. Individual clinical judgment. c. If conventional lights are not able to lower the TSB, the possibility of hemolytic jaundice should be considered. Intensive phototherapy may have to be used in such situations. Phototherapy can be suspended when TSB levels fall below 15 mg/dl. Routine serum bilirubin estimation to see the rebound is usually not necessary but should be individualized. d. The lack of intensive phototherapy has been defined as inability to observe a decrease in the TSB @ 1-2 mg/dl for 4-6 hours and maintain the levels of the TSB below the exchange range. e. If the baby has high bilirubin levels, put the baby under intensive phototherapy and prepare to exchange blood transfusion. If intensive phototherapy does not reduce the levels of the TSB, blood transfusion should be exchanged. The upper TSB level in a baby from 25 to 48 h can indicate hemolytic disease. a. Intial jaundice 24 hours is always abnormal and should be investigated for the cause and may require aggressive management in the form of phototherapy and/or exchange transfusion. b. Individual clinical judgment. c. If conventional lights are not able to lower the TSB, the possibility of hemolytic jaundice should be considered. Intensive phototherapy may have to be used in such situations. Phototherapy can be suspended when TSB levels fall below 15 mg/dl. Routine serum bilirubin estimation to see the rebound is usually not necessary but should be individualized. d. The lack of intensive phototherapy has been defined as inability to observe a decrease in the TSB @ 1-2 mg/dl for 4-6 hours and maintain the levels of the TSB below the exchange range. e. If the baby has high bilirubin levels, put the baby under intensive phototherapy and prepare to exchange blood transfusion. If intensive phototherapy does not reduce the levels of the TSB, blood transfusion should be exchanged. The upper TSB level in a baby from 25 to 48 h can indicate hemolytic disease. 2. Newborn Rh Hemolytic Disease Since a significant proportion of deliveries are still occurs at home, Rh isoimmuniza-tion is an important public health problem in India(1-3). These babies can present as hydrops in birth if the awareness has been severe enough or so rapid increase or Seriously high TSB. Progressive anemia and hepato-splenomegaly are usually present. The peripheral look shows evidence of hemolisi in form of aniso-poikilocytosis, elevated normblasts and fragmented red cells. Babies are usually the positive reticulocyte of Coomb is High. The management of an immunitarian hydrops is a real challenge. Effective management requires a team approach for obstetricians and neonatologists that start from early pregnancy. Detailed discussion management of inmunitary hydrops is beyond the current scope communication. Babies, which are not hydropics, should have TSB and PCV measurement of cord blood in addition to ABO writing and Coomb test. In the case of severe anemia (PCV) partial blood is exchanged transfusion with 50 ml/kg red blood cells packed should be transported out for the rapid correction of anemia. Double volume of blood exchange transfusion is performed if other criteria are met. The TSB should monitoring closely every 8-12 hours and babies should be administered aggressive use of intensive phototherapy(17) (Table III). High-dose intravenous immunoglobulin (IGI) when given early in the course of disease can modify the course of the disease. When given in dose of 0.5-1 g/kg as single dose, reduces hemolisi significantly and minimizes the need for transfusion of exchange and duration of phototherapy(18.19). Developing countries like ours, where Rh iso-inmunization still exists, provide an ideal scenario for conduct a randomized controlled study to show efficiency and safety IVIG therapy in Isoimmunized neonates Rh.3. ABO Incompatibility With decreased incidence of hemolytic disease Rh, The incompatibility ABO has become an important cause of hemolytic jaundice in newborn(1-3). In the blood group, the isohaemagglutin mother (Anti A) and Anti B) of type IgG cross the placenta and destroy type A or B red blood cells of the fetus. These isohaemagglutinas are of class IgG and differ from the usual IgM class isohaemagglutinas (incapable of crossing usually present in the blood (Anti A in blood group B and Anti B in blood group A). It is observed that hemolisi is more pronounced in Babies with blood group 'A' than 'B'. In incompatibility, ABO, hemolisi is generally less severe compared to Rh incompatibility and present most times after 24 hours of age. Pre-sence of setting does does not mean incompatibility, therefore the evidence of hemolisis must be carefully searched by examining the peripheral look and performing I reticulate to count. Coomb's direct test is generally nega-tive(13). The Table IV summarizes the suggested management of ABO incompatibility. Table III__Management of Rh hemolytic Disease of Newborn(17) A. Principles Exchange Blood Transfusion 1. Cord bilirubin 35 mg/dl 2. Cord Hb 10 mg/dl 3. In the event of severe awareness to eliminate antibodies in the baby (suggestion of severe affection, Coomb's indirect titre rose in the mother, positive direct proof of Coomb in the baby). B. Transfusion of later exchange 1. Age (h) TSB (mg/dl) 24 3 10 25-48 3 15 " No. 48 " 3 20 2. When the serum increase rate bilirubin 3 0.5 mg/dl per hour C. Intensive Phototherapy: Indicated at a bilirubin level, which is 5 mg/dl less than blood transfusion exchange. D. Preterm/Low birth weight babies: correspondingly lower values should be used. A level equal to or greater than 0.5 and 1% of the birth weight can be used as a rough guide for phototherapy and blood transfusion exchange, respectively. 4. Other hemolytic conditions Lower blood group incompatibility, G-6-PD deficiency, hereditary spherocytosis, autoimmune hemolytic anemia other causes of hemolytic jaundice. Of these deficiencies, G-6-PD deserves a special mention. G-6-PD deficiency is a common condition India, the incidence varies between 5-20% among different ethnic groups (1.2.20). It is more common in Tribes and Parsis. The jaundice can present at any time during the neonatal period, whether spontaneous or next exposure to oxidative stress. The physiological basis for excess no jaundice has been established in infants with G-6-PD deficiency. Increased breakdown of erythrocytes and reduction of bilirubin glucuronidation caused by defective G-6-PD activity in the hepato-cite may have a role in the pathogenesis(21). It can be severe enough to require exchange Blood transfusion (1,2). All babies who develop hyperbilirrubibinemia should :: A review of the deficiencies of the G-6-PD in family counselling with respect to the avoidance of harmful drugs in later life. Table IV_ Management of ABO Incompatibility Table IV_ Management of ABO Incompatibility Intervention TSB (mg/dl) Phototherapy 315-17 Exchange blood transfusion 20 Use the correspondingly low level for premature babies. 5. Premature levelsBilirubin for intervention have been reported before in infants with standard risk and high risk(22). High risk Babies are those who have birth weight of less than 1500 g, hypothermia, asphyxiation, acidosis, hypo-albuminemia, sepsis, meningitis, or administer drugs that have potential to displace the bilirubin of the albumin. In high-risk infants cut for intervention are lower. Like a broad blood transfusion guide exchange was recommended for babies bilirubin level of 1% of body weight in grams, i.e. for a baby with wieght of birth 1700 g bilirubin level for exchange is 17 mg/dl. There is change in the induced bilirubin spectrum brain damage in premature babies with virtual disappearance of kernicterus in modern neonatal units in the West. New evi-dences suggest low bilirubin kernicterus in the 1970s and 1980s, which formed the basis for such a recommendation was probably due to the nature of support and UCIN practices such as the use of sulfisoxozale and benzyl alcohol. In addition, in neuro-development follow-up studies, hyper-bilirrubibinemia has not emerged as a single risk factor for the poor neurological outcome(23). There has recently been a change in management practices hyperbilirubinemia in premature babies in the form of starting intervention at higher levels(24). Table V refers to weight-based cut for Phototherapy and transfusion exchange. These are approximate guidelines. It has been recommended that each baby be individualized for intervention.6. Restricted baby treatmentBilirubin is related to maturity the hepatobiliary system and, therefore, in deciding the intervention, The gestational age should be taken into account more than weight.7. Breastfeeding studies in the last two decades have found increased incidence of hyperbilirubibinemia in breast-feeding babies. In of Carvalho et al.(25) reported that the frequency of Food was crucial in the genesis of neonatal hyperbilirubinemia. More Progressive breastfeeding led to a lower incidence of jaundice. These are Researchers also showed that glucose water or water supplementation in breastfeeding infants gives rise to a greater serum bilirubin Concentrations that do not supplement infants(26). Yammauchi et al. reported that infants who breastfeed more often milk and less weight loss(27). The degree of jaundice on the 6th day inverse correlational age with frequency of feeding in the first 24 hours. In a recent study(28) the role of breastfeeding in jaundice that occurs in first week showed a statistically significant positive correlation among patients with TSB ratio12.9 mg/dL and supplementary feeding. Infants did not have a greater frequency of significant hyperbilirubinemia but a very small subpopulation had high bilirubin level. Weight loss was strongly associated considerably hyperbilirubi-nemia and was more pronounced in babies with mixture feeding instead of those in exclusive breastfeeding. A well-designed longitudinal study on the physiological jaundice pattern in optimal Breastfeeding still lacks. But it feels like exaggeration jaundice in breast-feeding babies is due to inadequate ingestion of milk and calories instead of any ingredient in breast milk itself exaggerating jaundice. In babies with optimal breast milk, the pattern should not vary and exaggeration is probably related to non-physical-logic management breastfeeding. So while they manage these babies, frequent and exclusive Breastfeeding should be low in consumption. Table V__ Management of neonatal hyperbili-rubinemia in very low-weight babies at birth Based on the level of Bilirubin (mg/dl)(24) Table V__ Management of neonatal hyperbili-rubinemia in very low-weight babies at birth Based on the level of Bilirubin (mg/dl)(24) Weight (g) Phototherapy Consider the exchange blood transfusion 500- 750 5-8 12-15 750-1000 6-10 √ 13 1000-1250 8-10 15-18 1250-1500 10-12 17-20 a. These are guidelines; each baby must be individualized. b. As a rough guide, start phototherapy in a well-VLBW baby if bilirubin levels are about 1% of the birth weight and exchange blood transfusion to a higher value of more than 5 g/dl. A sick VLBW baby requires intervention before. a. These are guidelines; each baby must be individualized. b. As a rough guide, start phototherapy in a well-VLBW baby if bilirubin levels are about 1% of the birth weight and exchange blood transfusion to a higher value of more than 5 g/dl. A sick VLBW baby requires intervention before. 8. Protracted jaundice No firm rules can be framed to define abnormalities persistence of jaundice in a newborn. It is common to see newborns significantly jaundiced even 2-3 weeks. Careful review of maternity baby's history and thorough clinical examination Adequate management guide (Table VI). According to AAP practice parameter, these babies should be investigated after three weeks, provided they are free of any disease, not having abnormal physical exam, dark urine or light stools(14). By the way, the most common cause of prolonged jaundice is called ñustmilk jaundice ' (BMJ). These babies can be handled effectively with the continuation of breastfeeding and phototherapy even if the TSB exceeds 20 mg/dl in a term Baby. It is important that you do not stop breastfeeding routinely in these babies, which is of immense benefit to the baby(29). Stop. breastfeeding, even for short duration, will result in anxiety and resulting removal of breastfeeding in the mother and many babies can do not return to exclusive breastfeeding. Besides, this extends to Wrong message about breastfeeding. Guidelines have recently been established established for the management of infants with extended conjugate hyperbilirubinemia (30). E. Therapeutic interventions E. Therapeutic Interventions (i) Blood Transfusion Exchange Exchange Exchange Exchange Exchange (ET) is an effective method lowering very high bili-rubin. Blood transfusion early exchange reverts the brain damage of transient bilirubin(31). Abnormal auditorium evoked chronology in case of neonatal hyperbilirubinemia that persists even after well-connected therapy with neuro-developmental delay at 1 year of age(32). Fresh blood, preferably 72 hours of age are used. For the choice of blood see the table VII. The procedure is performed by a catheter of 5 or 6 F in umbilical vein for a distance where you get free flow of blood. In In addition to the risk of blood birth infection, ET carries a significant risk of vascular accident morbidity, heart complications and biochemical or hematological disorders, although mortality due to procedure itself is very rare (1,3,33). Table VI_Prolonged ictericia Table VI_Prolonged ictericia Common causes 1. Maternal milk jaundice 2. Extravaded blood, for example, cefalhematoma 3. Persistence of hemolisis 4. Deficiency of the G-6-PD 5. Hipotiroidism Workup • Careful history and clinical examination • Regulate the colostasis (color of stool, direct and indirect bilirubin levels) • Find hemolisis, G-6-PD display • discard hypothyroidism • Extends urinary tract infection (ii) Phototherapy Phototherapy has been found effective in treatment of hyperbilirubibinemia in hemolytics, as well as non-hemolytic Adjustments. It has drastically reduced the need for transfusion of exchange. The TSB decrease depends on the dose of radiation, skin area TSB level exposed and initial. The bilirubin not conjugated in the skin converted into water-soluble photoproducts on exposure to light particular wavelength (425-475 mm). These photo-products are water soluble, non-toxic and excreted in intestine and urine. For phototherapy to be effective, bilirubin needs to be present on the skin so not paper for prophylactic phototherapy(24). (a) Isomerization of configuration: Here. bilirubin Z-isomers become E-isomers. The reaction is instant about exposure to light but reversible as bilirubin Get to the bile duct. After the exhibition of 8-12 hours Phototherapy, this constitutes about 25% of the TSB, which is not toxic. Since this is slowly excreted from the body, so this is not a problem Mecha-nismo for the TSB decrease. (b) Structural Isomerization: This Is an irreversible reaction where bilirubin becomes Lumirubin. The reaction is directly proportional to the dose Photo therapy. This product forms 2-6% of the TSB that is quickly excreted from the body and is primarily responsible for induced phototherapy decline on the TSB. c) Photo oxidation: This is a minor Reaction, where the photoproducts excrete in the urine. (a) Isomerization of configuration: Here. bilirubin Z-isomers become E-isomers. The reaction is instant about exposure to light but reversible as bilirubin Get to the bile duct. After the exhibition of 8-12 hours Phototherapy, this constitutes about 25% of the TSB, which is not toxic. Since this is slowly excreted from the body, so this is not a problem mecha-nism for decrease in TSB.(b) Structural Inomerization: This is an irreversible reaction where bilirubin becomes Lumirubin. The reaction is directly proportional to the dose Photo therapy. This product forms 2-6% of the TSB that is quickly excreted from the body and is primarily responsible for induced phototherapy TSB decline.(c) Photo oxidation: This is a minor Reaction, where the photoproducts excrete in the urine. Table VII__ Election of Blood for Blood Transfusion Table VII__ Election of Blood for Blood Transfusion Rh iso-immunization: In emergency situations use negative O Rh cells. Ideal is to use negative blood O Rh suspended in AB plasma. The blood group of the baby paired cross, but Rh negative can also be used. ABO Incompatibility: Blood group or types (Rh compatible) with baby. Ideal to use the blood group O (Rh compatible) suspended in AB plasma. Other situations: Cross-Birth Blood Group. Blood volume used: For partial exchange: 50 ml/kg For double volume exchange: twice the baby's blood volume. Types of Light The most effective lights are those that have high-energy output near peak adsorption of bilirubin (450-460 nm). Blue special lamps with maximum output to 425-475 nm the most efficient and these do not emit harmful ultraviolet rays. Blue Green light can interfere with the monitoring of cyanosis. Plus, blue light causes nausea, gin and headache to staff working in ICU. The green light causes the erythema and the subsequent tanning of the skin. A combination of two blue and two white tube lights (20 w each) are sufficient to provide an adequate irradiation of 4 to 8 microwatt/cm2/nm. Increase radiation to 10-12 microwatt/cm2/nm a combination of four blue tubes and two whites have to be used. The Radiation should be measured by the fluximeter(34). Fresh day light bulbs ( fluorescent tube light 6-8, 20 W each) with a main peak of 550 to 600 nm and a range of 380 to 700 nm are most commonly used in phototherapy units in our country. These units provide 4-6 microwatt/cm2/nm, when fluorescent tubes are new. With the use of irradiancy is tied to be much lower than required for therapeutic purposes. These units are effective in the treatment of non-hemolytic jaundices in the term and premature Newborns. Occasionally these are not particularly effective in cases of severe or rapidly increasing neonatal jaundice. Remember the lamps should be changed every 3 months or before if the irradian is being monitored. Putting a blue or glass plastic sheet in front of white lamps will not increase the irradiation of the unit in the bluegreen range, but rather decrease. In an attempt to offer intensified phototherapy; Carvalho et al. designed a unit with seven-day fluorescent light tubes placed immediately under the floor of a transparent Plexiglas crib(35). The unit delivered an irradiation of 19 μw/cm2/nm and was as effective as a unit containing special blue fluorescent tube in treatment of non-hemolytic hyperbilirubinemia in infants. Halogen white light (150 W, 21 V) that has significant The output in the blue spectrum is useful for babies under radiant heaters. Opening size (3-20 inches) and mattress distance drive can be controlled. The interior coating of reflective surface of the halogen bulb absorbs most of the infrared rays (IR) (a fan continuously cools it) and a UV Filter in front of blocks of light bulbs harmful UV rays from reaching the baby. The indigenous halogen bulb phototherapy units may lack UV filter and therefore may not be safe for use(34). The recent fiber optic light system provides high-intensity lamp light to a fiber optic pad or blanket. Lighting is transmitted from a halogen lamp source to a fiber optic package contained in a pad in which the baby can lie. These systems have obvious advantages of not requiring eye patch, don't warm the baby; the team is less voluminous than conventional phototherapy equipment and babies can be maintained and nurses while receiving photo therapy. Available studies(36) have shown that fiber optic system is as effective as conventional phototherapy systems in short-term and premature babies. Double surface phototherapy is more effective than the single surface because the average irradiation of the previous is greater(37). Double surface phototherapy can be provided either by special blue light of double surface or by conventional blue Light fiber and subsurface phototherapy. This is convenient. way to offer double phototherapy when it is necessary to reduce the bilirubin level as fast as possible. A new high-intensity nitronic blue light emitting diode phototherapy has recently been tested and found effective in reducing bilirubin by providing much greater irradiation Intensive phototherapy(38). It's a mistake to assume that only because of a Phototherapy unit emits fluorescent light when activated; is necessarily the treatment for the baby with jaundice. In a audit of fetotherapy units in four neonatal centres care in different parts of the country, it was found that only 31% (18/50) units provided an acceptable level of irradiation (39). That's right. imperative that one must periodically verify the irradiation of photo therapy units used to treat pathological jaundice. Phototherapy used for treating pathological jaundice is like giving a medicine. One not. justified in the use of substandard light sources for the treatment of neonatal jaundice. Solar light is relatively ineffective due to low blue content of light. In addition, hyper-piraxia and skin burns can occur in prolonged periods exposure to sunlight. Phototherapy has been used for 50 years and has showed excellent safety track. Recently, the effect of phototherapy on The rate of cerebral blood flow (CBFV) has been reported. Phototherapy increase of average CBFV in all premature babies, who returned to pre-therapy values after discontinued phototherapy only in Non-ventilated babies(4). Even in short-term babies, phototherapy increased CBFV, which returned to the pre-therapy level after the interruption of Phototherapy(41). Phototherapy has been shown to affect the short term behaviour of the term infant, which has been attributed to maternity separation(42). So one should encourage the mother to breastfeed and interact with your baby regularly. In addition, the influences of phototherapy cytokine production by perpheral mononuclear blood cells(43). Phototherapy also has photoxidative effects on intravenous lipids, proteins and drugs such as anphotericin B. F. Drug treatment F. Pharmacological treatment(i) PhenobarbitonePhenobarbitone has been in use for a long time to prevent jaundice. Induces glucuronyl transferase enzyme so it improves conjugation and absorption and excretion of bilirubin by liver cells. Although their use has not become the standard of care from now on, there the evidence that phenobarbitone can be useful prevention is increasing measurement, especially in preterms(44), hemolytic setting and in case of extravagant blood. If used in doses of 5-10 mg/kg/day, you may have beneficial effect without significant adverse effects.(ii) High Dose Intravenous ImmunoglobulinHyperbilirubinemia in Rh and ABO sensitized of the destruction of neonatal red cells covered by transplacental acquired antibodies that causes the destruction of red cells mediated by Fc receptor bearing cells within the reticuloendothelial system. Recent studies have shown that high intravenous dose Immunoglobulin therapy is effective in modifying hyperbilirubinemia in most cases of positive hemolytic anemia of Coomb(18,19). It was. proposed that immunoglobulin blocks Receptors Fc inhibiting this hemolysis and reduction of bilirubin training. Intravenous immunoglobulin is given in doses of 500-1000 mg/kg as slow infusion over 2 hours. The child must be carefully monitored so that it is possible effects with special attention to heart rate and blood pressure.(iii) ProtoporfirinsMetalloporphyrins are competitive heme inhibitors oxygenase, an enzyme that limits the rate in heme catabolism by reducing this Production of bilirubin. Clinical trials have shown that the tin Mesoporfirins (SnMP) suppresses bilirubin production. The drug has been found to be devoid of greater negative effect, the only transitory being It's very bad. SnMP at a single dose of 6 μmol/kg tested plus effective phototherapy in a group of infants in the short term without hemolytic disease (45). Recently a similar study on the term infants without hemolytic disease also showed the ability to SnMP to abolish the need for phototherapy(46). To date, SnMP remains experimental but seems to have a promise for the future. In conclusion, non-conju management hyperbilirubinemia in newborns has undergone changes based on appearance tests. New approaches to preventing bilirubin brain damage are on the horizon, but phototherapy and blood transfusion exchange are the most used modalities to reduce serum bilirubin levels. Early prediction of "at risk" baby development of significant jaundices is gaining attention and interest Pediatricians. This issue is particularly relevant in the context of the principles hospital discharge policy in developing countries where there is resource shortage. Collaborators: The AKD provided the general framework and concept of the article. He will. act as the guarantor of the paper. RA collected data and wrote manuscript, which was edited by AKD. Financing: None. Competing interests: None. Key messages • Unconjugated jaundice is important problem in newborns. • Hyperbilirubinemia in healthy term Babies can be given according to AAP criteria. There is growth consensus on the use of higher bilirubin levels for intervention in premature babies. • Phototherapy is an effective modality for the treatment of hyperbilirubinemia in non-hemolytic as hemolytic configuration. • Fenobarbitone, intravenous immunoglobulin and Sn-protoporfirins are the pharmacological measures that show Promise. Key messages Key messages • Unconjugated jaundice is important problem in newborns. • Hyperbilirubinemia in healthy term Babies can be given according to AAP criteria. There is growth consensus on the use of higher bilirubin levels for intervention in premature babies. • Phototherapy is an effective modality for the treatment of hyperbilirubinemia in non-hemolytic as hemolytic configuration. • Fenobarbitone, intravenous immunoglobulin and Sn-protoporfirins are the pharmacological measures that show Promise. • Unconjugated jaundice is important problem in newborns. • Hyperbilirubinemia in healthy term Babies can be given according to AAP criteria. There is growth consensus on the use of higher bilirubin levels for intervention in premature babies. • Phototherapy is an effective modality for the treatment of hyperbilirubinemia in non-hemolytic as hemolytic configuration. • Fenobarbitone, intravenous immunoglobulin and Sn-protoporfirins are the pharmacological measures that show Promise. References 1. Narang A, Gathwala G, Kumar P. Neonatal jaundice: Analysis of 551 cases. Indian Pediatr 1997; 34: 429-432. 2. Singhal PK, Singh M, Paul VK, Deorari AK, Ghorpade MG. Neonatal hyperbilirubibinemia: An Analysis 454 cases. Indian Pediatr 1992; 29: 319-325. 3. Bahl L, Sharma R, Sharma J. Ethology of Neonatal jaundice in Shimla. Indian Pediatr 1994; 31: 1275-1278. 4. Cashore WJ. Bilirubin Metabolism and Toxicity in the newborn. In: Fetal and neonatal physiology, 2nd edition. Eds Polin RA, Fox WW. Philadelphia. W.B. Saunders Company, 1998; pp 1493-1497. 5. Bhutani VK, Johnson L, Sivieri EM. Predictive ability of an hour of specific bilirubin predisposition for later significant hyper-bilirubinemia in healthy term and near term newborns. Pediatrics 1999; 103-6-14. 6. Alpay F, Sarici SU, Tosuncuk HD, Serdar MA, Inanc N, Gokcay E. The value of the first day bilirubin measurement prediction of the development of significant hyperbilirubinemia term healthy newborns. Pediatrics 2000; 106: e16. 7. Awasthi S, Rehman H. Early prediction Neonatal hyperbilirubinemia. Indian J Pediatr 1998; 65: 131-139. 8. Stevenson DK, Vreman JH. Carbon monoxide and Production of bilirubines in neonates. Pediatrics 1997; 100: 252-254. 9. Tan KL. transcutaneous bilirubinomy in its entirety Chinese and Malaysian children. Acta Pediatr Scand 1982; 71: 593-596. 10. Jacques S, Saidi I, Ladner A, Oerlberg D. Develop a fiber optic re-election spectrometer to monitor bilirubinemia in neonates. SPIE Proceedings 2975, Laser Tissue Interactions, San José CA, February 1997; p7. 11. Bhutani VK, Gourley GR, Adler S, Kreamer B, Dalm C, Johnson LH. Non-invasive measurement of total serum bilirubin in a population of newborns pre-load multiracial Assess the risk of severe hyperbilirubinemia. Pediatrics 2000; 106: e17. 12. Lodha R, Deorari AK, Jatana V, Paul VK. Non-invasive estimation of total serum bilirubin by multiple wavelength Spectral reflectance in the neonates. Indian Pediatr 2000; 37: 771-775. 13. Simpson L, Deorari AK, Paul VK. Cord bilirubin as pathological icterity predictor – A cohort study (low publication). 14. American Academy of Pediatrics. Practice parameter: Handle of hyperbilirubi-nemia in term healthy Newborn. Pediatrics 1994; 94: 558-567. 15. Maisels MJ, Newman TB. Kernicterus in otherwise healthy, newborn breasts. Pediatrics 1995; 96: 730-733. 16. Moyer VA, Ahn C, Sneed S. Accuracy of clinical trial in the neonatal period. Arch Pediatr Adolesc Med 2000; 154: 391-394. 17. Maisels MJ. Jaundice. In: Neonatology: Patophysiology and Management of the Newborn, 4th edn. Eds Avery GB, Fletcher MA, McDonald MG. Philadelphia, J.B. Lippincott, 1994; p 765. 18. Alpay F, Sarici SU, Okutan V, Erden G, Ozean-O, Gokcay E. High-dose intravenous immunoglobulin therapy in neonatal immune hemolytic jaundice. Acta Pediatr 1999; 88: 216-219. 19. Agarwal R, Seth R, Paul VK, Deorari AK. High intravenous dose of immunoglobulin therapy in the treatment of Rhesus Hemolytic disease. J Trop Ped, April 2002 (In Press). 20. Singh M. Jaundice. In: Watch out Newborn, 5th edn. New Delhi. Sagar Publications, 1999; pp 245-266. 21. Seidman DS, Shildr M, Stevenson DK, Vreman JH. Function of hemolysis in neonatal jaundice associated with Glucose-6-Phos-phate Dehydrogenase deficiency. J Pediatr 1995; 127: 804-806. 22. National Institute of Child Health and Human Development. Random controlled phototherapy test for Neonatal hyperbilirubinemia. Pediatrics 1985; 75 (Supplement): 385-441. 23. Watchko JF, Oski FA. Kernicterus in default newborns: Past, present and future. Pediatrics 1992; 90: 707-715. 24. Cashore WJ. Bilirubin and jaundice in the micropremie. Clin Perinatol 2000; 27: 171-179. 25. De Carvalho M, Hall M, Marvey D. Effect of supplementation of water in physiological jaundice in breast-feeding babies. Arch Dis Child 1981; 56: 569-569. 26. De Carvalho M, Klaus MH, Merkatz MB. Breastfeeding frequency and serum bilirubin concentration. Am J Dis Child 1982; 136: 747-748. 27. Yamauchi Y, Yamanouchi H. The relationship between the variables of accommodation/no room and lactation. Acta Pediatr Scand 1990; 79: 1017-1022. 28. Bertini G, Dani C, Tronchin M, Rubaltelli FF. Does breastfeeding really favor neonatal jaundice? Pediatrics 2001; 107: e41. 29. Gartner LM, Lee K. Jaundice in breastfed infants. Clin Perinatol 1999; 26: 431-445. 30. Yaccha SK. Neonatal consensus reports Coltasis. Indian Pediatr 2000; 37: 845-851. 31. Deorari AK. Singh M, Ahuja GK, Bisht MS, Verma A, Paul VK, Tandon DA. One-year result of serious babies neonatal hyperbilirubinemia and reversible abnormality in the brain stem evoked hearing responses. Indian Pediatr 1994; 31: 915-921. 32. Agarwal VK, Shukla R, Misra PK, Kapoor RK, Malik GK. Hearing brain evokes newborn response hyperbilirubinemia. Indian Peidatr 1999; 35: 513-518. Jindal B, Narang A, Das R. Post transfusion graft against host disease: A recognized entity. Indian Pediatr 2001; 38: 179-183. 34. Agarwal RK, Deorari AK. Neonatal jaundice. Indian Pediatr 1999; 36: 110-112. 35. Carvalho MD, Carvalho DD, Trzmielina S, Lopes JMA, Hansen TWR. Intensified phototherapy with daylight fluorescent lamps. Clin Pediatr 1999; 88: 768-771. 36. Costello SA, Nyikal J, Yu VVH, McCloud P. bili blanket phototherapy system versus conventional phototherapy. A randomized control test in premature babies. J Pediatr Child Health 1995; 31: 11-31. 37. Sarici SV, Alpay F, Unay B, OZcan O, Gokcay E. Double versus individual phototherapy in newborns in the term Significant hyperbilirubinemia. J Trop Pediatr 2000; 46: 36-39. 38. Sedman DS, Moise J, Ergaz Z, Laor A, Vreman HJ, Stevenson DK et al. A new blue light emitting Phototherapy device: A possible randomized controlled trial. J Pediatr 2000; 136: 771-774. 39. Pejaver RK, Vishwanath J. An audit of Phototherapy units. Indian J Pediatr 2000; 67: 883-884. 40. Benders MJ, Van Bel F, Van de Born. The phototherapy effect on the speed of cerebral blood flow in default infants. Biol Neonate 1990; 73: 228-234. 41. Benders MJ. Van Bel F, Vande-BorM. Hemodynamic consequences of phototherapy in short-term babies. Eur J Pediatr 1999; 158: 323-328. 42. Abrol P, Sankarasubramanian R. Effect of Phototherapy on the behavior of the Jaundic neonates. Indian J Pediatr 1998; 65: 603-607. 43. Sirota L, Straussbery R, Gurrary N, Aloni D, Bessler H. Phototherapy for neonatal hyperbilirubinemia affects cvytokine production by peripheral blood mononuclear cells. Eur J Pediatr 1999; 158: 910-913. 44. Kumar R, Narang A, Garewal G. Prophylactic phenobarbitone for neonatal jaundice in babies from 1000 to 1499 grams. XXth Annual Convention of the National Forum of Neonatology, Mumbai, 3-5 November 2000. 45. Kappas A, Drummond GS, Henschke C, Valaes T. Direct comparison of Sn Meso-porfirins, bilirubin inhibitor production and phototherapy in hyperbili-rubinemia control of newborns in the short term. Pediatrics 1995; 95: 468-474. 46. Martinez JC, García HO, Otheguy LE, Drummond GS, Kappas A. Control of severe hyperbilirubinemia in long-term newborns with the bilirubin production inhibitor Sn-Mesoporphyrins. Pediatrics 1999; 103: 1-5. 1. Narang A, Gathwala G, Kumar P. Neonatal jaundice: Analysis of 551 cases. Indian Pediatr 1997; 34: 429-432. 2. Singhal PK, Singh M, Paul VK, Deorari AK, Ghorpade MG. Neonatal hyperbilirubibinemia: An Analysis 454 cases. Indian Pediatr 1992; 29: 319-325.3. Bahl L, Sharma R, Sharma J. Ethology of Neonatal jaundice in Shimla. Indian Pediatr 1994; 31: 1275-1278.4. Cashore WJ. Bilirubin Metabolism and Toxicity in the newborn. In: Fetal and neonatal physiology, 2nd edition. Eds Polin RA, Fox WW. Philadelphia. W.B. Saunders Company, 1998; pp 1493-1497.5. Bhutani VK, Johnson L, Sivieri EM. Predictive ability of an hour of specific bilirubin predisposition for later significant hyper-bilirubinemia in healthy term and near term newborns. Pediatrics 1999; 103-6-14.6. Alpay F, Sarici SU, Tosuncuk HD, Serdar MA, Inanc N, Gokcay E. The value of the first day bilirubin measurement prediction of the development of significant hyperbilirubinemia term healthy newborns. Pediatrics 2000; 106: e16.7. Awasthi S, Rehman H. Early prediction Neonatal hyperbilirubinemia. Indian J Pediatr 1998; 65: 131-139.8. Stevenson DK, Vreman JH. Carbon monoxide and Production of bilirubines in neonates. Pediatrics 1997; 100: 252-254.9. Tan KL. transcutaneous bilirubinomy in its entirety Chinese and Malaysian children. Acta Pediatr Scand 1982; 71: Jacques S, Saidi I, Ladner A, Oerlberg D. Develop a fiber optic re-election spectrometer to monitor bilirubinemia in neonates. SPIE Proceedings 2975, Laser Tissue Interactions, San José CA, February 1997; p7.11. Bhutani VK, Gourley GR, Adler S, Kreamer B, Dalm C, Johnson LH. Non-invasive measurement of total serum bilirubin in a population of newborns pre-load multiracial Assess the risk of severe hyperbilirubinemia. Pediatrics 2000; 106: e17.12. Lodha R, Deorari AK, Jatana V, Paul VK. Non-invasive estimation of total serum bilirubin by multiple wavelength Spectral reflectance in the neonates. Indian Pediatr 2000; 37: 771-775.13. Simpson L, Deorari AK, Paul VK. Cord bilirubin as pathological icterity predictor – A cohort study (low publication). 14. American Academy of Pediatrics. Practice parameter: Handle of hyperbilirubi-nemia in term healthy Newborn. Pediatrics 1994; 94: 558-567.15. Maisels MJ, Newman TB. Kernicterus in otherwise healthy, newborn breasts. Pediatrics 1995; 96: 730-733.16 Moyer VA, Ahn C, Sneed S. Acuracy of clinical trial in the neonatal period. Arch Pediatr Adolesc Med 2000; 154: 391-394.17. Maisels MJ. Jaundice. In: Neonatology: Patophysiology and Management of the Newborn, 4th edn. Eds Avery GB, Fletcher MA, McDonald MG. Philadelphia, J.B. Lippincott, 1994; p 765.18 Alpay F, Sarici SU, Okutan V, Erden G, Ozean-O, Gokcay E. High-dose intravenous immunoglobulin therapy in neonatal immune hemolytic jaundice. Acta Pediatr 1999; 88: 216-219.19. Agarwal R, Seth R, Paul VK, Deorari AK. High intravenous dose of immunoglobulin therapy in the treatment of Rhesus Hemolytic disease. J Trop Ped, April 2002 (In Press).20. Singh M. Jaundice. In: Watch out Newborn, 5th edn. New Delhi. Sagar Publications, 1999; pp 245-266.21. Seidman DS, Shildr M, Stevenson DK, Vreman JH. Function of hemolysis in neonatal jaundice associated with Glucose-6-Phos-phate Dehydrogenase deficiency. J Pediatr 1995; 127: 804-806.22 National Institute for Child and Human Health Development. Random controlled phototherapy test for Neonatal hyperbilirubinemia. Pediatrics 1985; 75 (Supplement): 385-441.23. Watchko JF, Oski FA. Kernicterus in default newborns: Past, present and future. Pediatrics 1992; 90: 707-715.24. Cashore WJ. Bilirubin and jaundice micropremie. Clin Perinatol 2000; 27: 171-179.25. De Carvalho M, Hall M, Marvey D. Effect of supplementation of water in physiological jaundice in breast-feeding babies. Arch Dis Child 1981; 56: 569-569.26. De Carvalho M, Klaus MH, Merkatz MB. Breastfeeding frequency and serum bilirubin concentration. Am J Dis Child 1982; 136: 747-748.27. Yamauchi Y, Yamanouchi H. The relationship between the variables of accommodation/no room and lactation. Acta Pediatr Scand 1990; 79: 1017-1022.28. Bertini G, Dani C, Tronchin M, Rubaltelli FF. Does breastfeeding really favor neonatal jaundice? Pediatrics 2001; 107: e41.29. Gartner LM, Lee K. Jaundice in breastfed infants. Clin Perinatol 1999; 26: 431-445.30. Yaccha SK. Neonatal consensus reports Coltasis. Indian Pediatr 2000; 37: 845-851.31. Deorari AK. Singh M, Ahuja GK, Bisht MS, Verma A, Paul VK, Tandon DA. One-year result of serious babies neonatal hyperbilirubinemia and reversible abnormality in the brain stem evoked hearing responses. Indian Pediatr 1994; 31: 915-921.32. Agarwal VK, Shukla R, Misra PK, Kapoor RK, Malik GK. Hearing brain evokes newborn response hyperbilirubinemia. Indian Peidatr 1999; 35: 513-518.33. Jindal B, Narang A, Das R. Mail Transfusion graft against host disease: A recognized entity. Indian Pediatr 2001; 38: 179-183.34. Agarwal RK, Deorari AK. Neonatal jaundice. Indian Pediatr 1999; 36: 110-112.35. Carvalho MD, Carvalho DD, Trzmielina S, Lopes JMA, Hansen TWR. Intensified phototherapy with daylight fluorescent lamps. Clin Pediatr 1999; 88: 768-771.36. Costello SA, Nyikal J, Yu VVH, McCloud P. bili blanket phototherapy system versus conventional phototherapy. A randomized control test in premature babies. J Pediatr Child Health 1995; 31: 11-31.37. Sarici SV, Alpay F, Unay B, OZcan O, Gokcay E. Double versus individual phototherapy in newborns in the term Significant hyperbilirubinemia. J Trop Pediatr 2000; 46: 36-39.38. Sedman DS, Moise J, Ergaz Z, Laor A, Vreman HJ, Stevenson DK et al. A new blue light emitting Phototherapy device: A possible randomized controlled trial. J Pediatr 2000; 136: 771-774.39. Pejaver RK, Vishwanath J. An audit Phototherapy units. Indian J Pediatr 2000; 67: 883-884.40. Benders MJ, Van Bel F, Van de Born. The phototherapy effect on the speed of cerebral blood flow in default infants. Biol Neonate 1990; 73: 228-234.41. Benders MJ. Van Bel F, Vande-BorM. Hemodynamic consequences of phototherapy in short-term babies. Eur J Pediatr 1999; 158: 323-328.42. Abrol P, Sankarasubramanian R. Effect of Phototherapy on the behavior of the Jaundic neonates. Indian J Pediatr 1998; 65: 603-607.43. Sirota L, Straussbery R, Gurrary N, Aloni D, Bessler H. Phototherapy for neonatal hyperbilirubinemia affects cvytokine production by peripheral blood mononuclear cells. Eur J Pediatr 1999; 158: 910-913.44. Kumar R, Narang A, Garewal G. Prophylactic phenobarbitone for neonatal jaundice in babies from 1000 to 1499 grams. XXth Annual Convention of the National Forum of Neonatology, Mumbai, 3-5 November 2000.45. Kappas A, Drummond GS, Henschke C, Valaes T. Direct comparison of Sn Meso-porfirins, bilirubin inhibitor production and phototherapy in hyperbili-rubinemia control of newborns in the short term. Pediatrics 1995; 95: 468-474.46. Martinez JC, García HO, Otheguy LE, Drummond GS, Kappas A. Control of severe hyperbilirubinemia in long-term newborns with the bilirubin production inhibitor Sn-Mesoporphyrins. Pediatrics 1999; 103: 1-5.

Neonatal Hyperbilirubinemia - Pediatrics - Merck Manuals Professional Edition

Newborn Baby Jaundice Bilirubin Levels Chart - Newborn baby

Normal Jaundice In Newborn Baby - newborn baby

Hyperbilirubinemia in the Term Newborn - American Family Physician

Newborn Baby Jaundice Level 17 - Newborn baby

Comparison of Bilirubin Levels in Newborns Receiving Blue and... | Download Table

Newborn Baby Jaundice Level Chart India - Newborn baby

Newborn Baby Jaundice Range - Newborn baby

Outcomes among Newborns with Total Serum Bilirubin Levels of 25 mg per Deciliter or More | NEJM

Transcutaneous Bilirubin Levels in the First 96 Hours in a Normal Newborn Population of ≥35 Weeks' Gestation | American Academy of Pediatrics

PDF) Methods for Determining Bilirubin Level in Neonatal Jaundice Screening and Monitoring: A Literature Review

Normal Jaundice In Newborn Baby - newborn baby
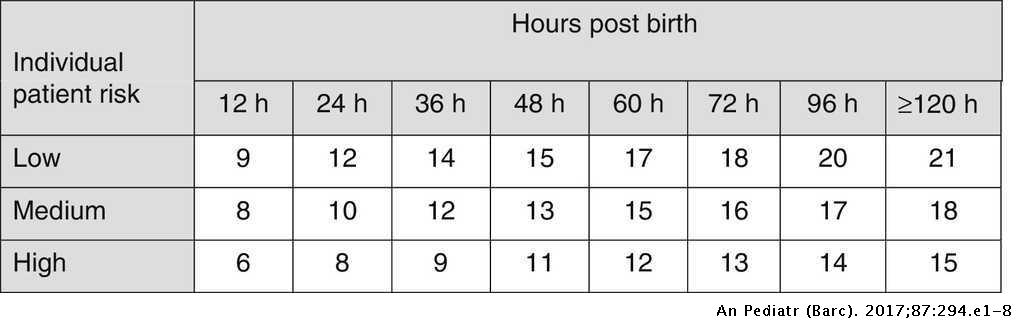
Guidelines for prevention, detection and management of hyperbilirubinaemia in newborns of 35 or more weeks of gestation | Anales de Pediatría

Transcutaneous bilirubin levels in a normal newborn population of 1 35... | Download Scientific Diagram

Newborn Baby Jaundice Bilirubin Levels Chart - Newborn baby

Relevance of the jaundice meter in determining significant bilirubin levels in term neonates at a tertiary hospital in Lagos State Oyapero O, Njokanma FO, Disu EA - Arch Med Health Sci

Visual Assessment of Neonatal Jaundice (Kramer's rule) | Neonatal, Jaundice newborn, Bilirubin newborns

Total Bilirubin Percentiles in the 223 Exclusively Breastfed Healthy... | Download Table

To study the prevalence of glucose 6 phosphate dehydrogenase(G6PD) deficiency in neonates with neonatal hyperbilirubinemia and to compare the course of the neonatal jaundice in deficient versus non deficient neonates Sinha R,

Correlation between bilirubin level 72 hours after birth and bodyweight... | Download Table
What Is Normal Level Of Jaundice In Newborn Babies - Newborn baby

PDF) The Effect of Massage on Serum Bilirubin Levels in Term Neonates with Hyperbilirubinemia Undergoing Phototherapy

Newborn Baby Jaundice Level Chart - newborn baby

Jaundice To Newborn Baby What Is The Level - Newborn baby

Transcutaneous Bilirubin Levels in the First 96 Hours in a Normal Newborn Population of ≥35 Weeks' Gestation | American Academy of Pediatrics

Newborn jaundice - BabyCenter India

Transcutaneous bilirubin levels in a normal newborn population of 1 35... | Download Scientific Diagram
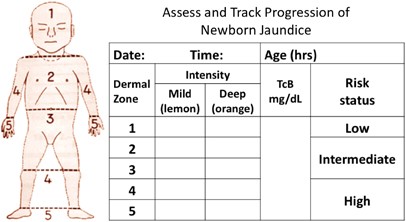
Universal bilirubin screening for severe neonatal hyperbilirubinemia | Journal of Perinatology

Percentile Values for TcB between 12 and 72 Hours | Download Table
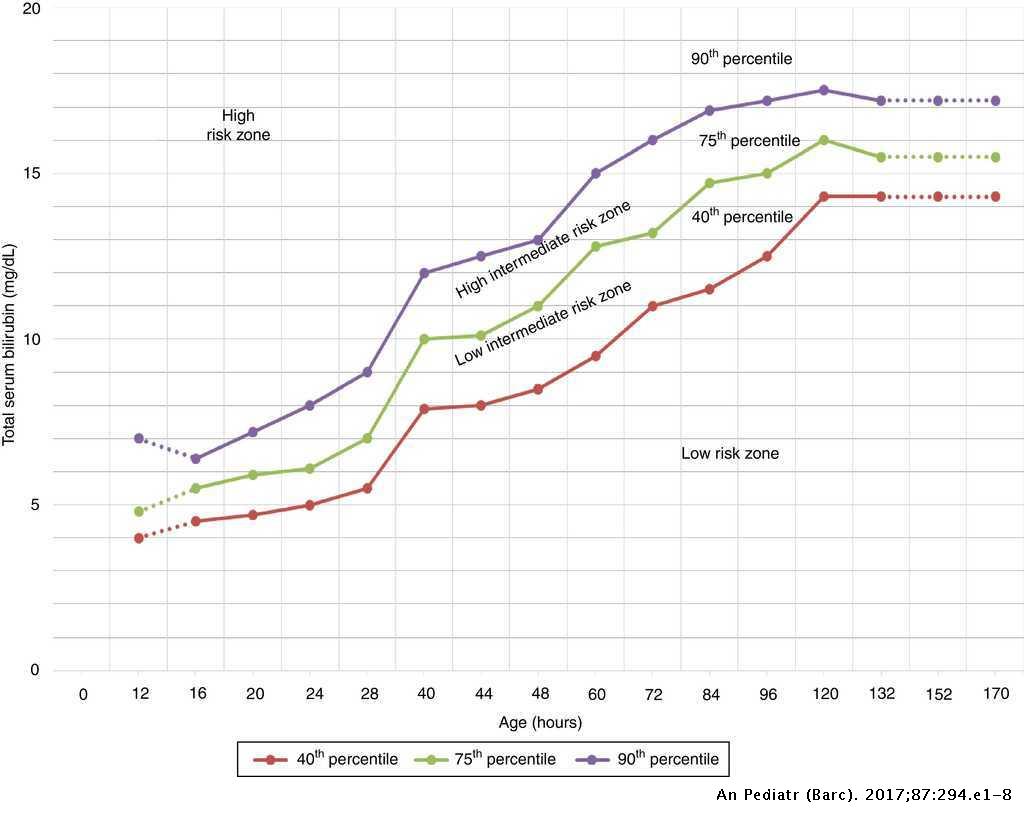
Guidelines for prevention, detection and management of hyperbilirubinaemia in newborns of 35 or more weeks of gestation | Anales de Pediatría

Hyperbilirubinemia in the Term Newborn - American Family Physician

Jaundice in Newborn Babies: Reasons, Signs & Treatment

Newborn Baby Jaundice Level 10 - Newborn baby

PDF) Jaundice in the Newborn

Variation in the serum bilirubin levels in newborns according to gender and seasonal changes

Bilirubin Test: Normal & High Bilirubin Levels in Adults & Newborns

Bilirubin Levels In Newborns - What's Normal? | BellyBelly

Outcome of neonates with severe hyperbilirubinemia in a tertiary level neonatal unit of North India - Clinical Epidemiology and Global Health

Jaundice in Newborns and Bilirubin Levels -- DrGreene.com

Transcutaneous Bilirubin Nomogram for Healthy Term and Late Preterm Neonates in First 96 Hours of Life
Posting Komentar untuk "normal bilirubin levels in newborns chart in india"